What is pilonidal abscess ?
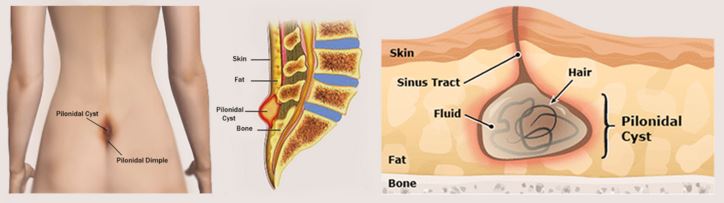
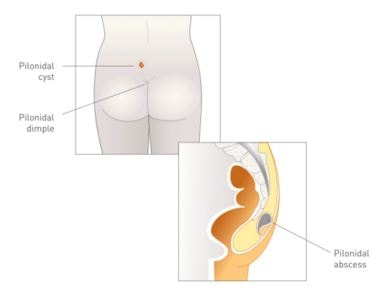
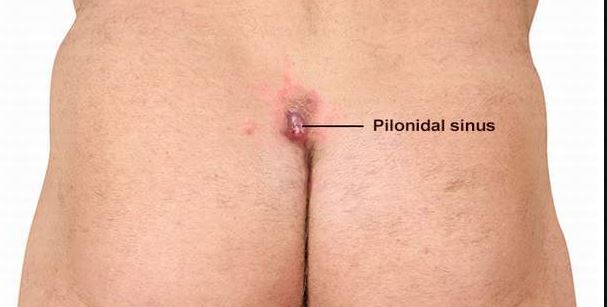
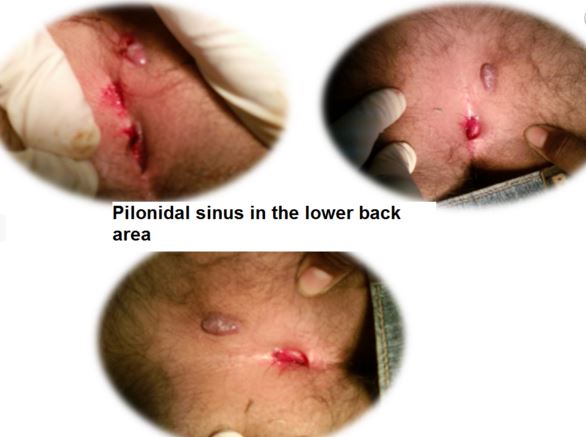
The pilonidal abscess is formed in between the cleft of the buttock, around 4-5 cm above the anus. The location of the abscess can also be described as the last segment of the spine i.e. in coccygeal region. The abscess is having debris along with hair growth.
The pilonidal abscess is asymptomatic, but if infection develops, then it become a painful cystic growth, pus is secreted with one or more opening present in the abscess wall. The one or more openings may present in the abscess for passing the pus. The incidence rate of pilonidal abscess is more in young male than female. Usually recurrence is common for pilonidal abscess.
It has been assumed that dilation of hair follicles causes penetration of a hair into the subcutaneous tissues. This condition occurs at latter part in the teenagers. Due to the hair follicle embedded in the skin, so it is not observed from outside, but a sinus is developed and responsible for promoting the hair penetration into the subcutaneous tissue. The abscess is formed due to foreign body or hair penetration.
The three mechanisms are responsible for pilonidal abscess formation:
- Invading hair
- pressure generates for hair penetration
- The susceptibility of the underlying subcutaneous tissue. (1,2)
Symptoms of pilonidal abscess
The following symptoms are common in pilonidal abscess, when it get infection:
- Pain at the tailbone (coccyx)
- Inflammation of the tailbone (coccyx)
- Redness
- Pus secretion
- Fever (1,2,3)
Causes
The cause of development of pilonidal abscess are slack fitted hair, skin and perineal flora.
38% patients have family history of pilonidal abscess, other risk factors are:
- Tight fitted cloth
- prolonged sitting
- Bicycle riding for prolong period
- The activity which promote friction of skin
All types of bacterial strains e.g., aerobic, anaerobic and mixed, are responsible for infecting the abscess and Staphylococcus aureus is the most common type of pathogen. (2)
Treatment
At the initial stage, warm sitz bath helps to provide relieve from pain. Proper hygiene and shaving is necessary for prevention of infection. In case of infection, it is suggested to consult doctors, they can prescribe broad spectrum antibiotics. (3,4,5)
Drainage
For relieving the symptoms, incision and drainage is very common option and perform in emergency department, need not to stay the patient in hospital. But drainage cannot prevent recurrence of pilonidal abscess. The process conducted in the following steps:
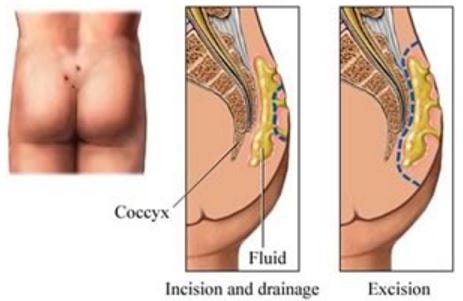
- Position the patient for conducting the procedure. Take care of his or her comfort and expose the area.
- Sometimes doctors recommend mild sedative, if patient become panic for conducting the process.
- Sterile technique is followed, to incision. Firstly wipe the place with Betadine solution. Local anesthetic is injected at the site for painless process.
- For opening the abscess cavity, sterile instruments are used and incision is made longitudinally and for drainage of the pus, the incision should deep up to subcutaneous layer of the skin.
- For complete removal of pus, blunt dissection may be applied depending upon the patient’s requirement and tolerance.
- After completion of the procedure, the sterile gauze and surgical tape needs to put in the place of the wound and analgesic is given to patient for pain management.
- Regular changing of dressing can help easy healing. (3)
Surgery
If the recurrence of pilonidal abscess is frequent with infection, then wide removal or removal and primary closure are used.
Wide Removal
For wide removal, surgeon is conducting the process with selecting wide range of the affected skin for cutting and removing the subcutaneous tissue layers. The opening of the wound is not closing for preventing the further infection. For dressing, wide gauze piece is used. The regular change in dressing is highly recommended for 4 to 6 months. The healing process is comparatively slow.
Removal and Primary Closure
In this process, after removal of the embedded hair and debris from the underlying subcutaneous tissue, the wound is stitched for fast healing. But chances of recurrence and infection is much more in this process.
Fibrin Glue
This is a novel technique, though the mechanism is same as removal and primary closure. In this process, newly invented fibrin glue is recommended for closing the wound, which need not to require changing of dressing. This technique give early healing and patient can go for routine work after a week.
Care after surgery
- Regular bathing with cleaning the affected place is require if the wound is open and required to dress with a gauze.
- If the wound is closed, then maintaining of dryness of the affected site is important, so keep away from water as doctor’s advice.
- Avoid soap water for cleaning purpose, as it may irritate the skin.
- Avoid any face powder
- Keep the place dry and remove wet dressing.
- For easy defecation, take plenty of fluid and roughage.(4,5)
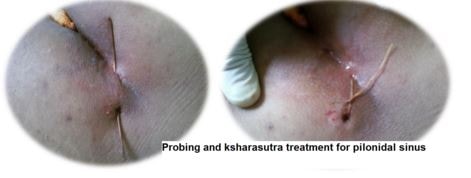
Pictures
References
1. Ramon A Riojas, Erik D Schraga et al (2015); Pilonidal Cystectomy; Retrieve from: http://emedicine.medscape.com/article/1830066-overview
2. Mayo Clinic Staff (2015); Pilonidal cyst; Retrieve from: http://www.mayoclinic.org/diseases-conditions/pilonidal-cyst/basics/definition/con-20025007
3. Michael D Lanigan, Gil Z Shlamovitz, et al. (2015), Pilonidal Cyst and Sinus Treatment & Management, Retrieve from: http://emedicine.medscape.com/article/788127-treatment
4. Debra Jaliman ( 2015), Medical Treatment for a Pilonidal Cyst; Retrieve from: http://www.webmd.com/skin-problems-and-treatments/guide/pilondial-cyst?page=2
5. Pilonidal sinus – Treatment (2014), NHS hospital services, Retrieve from: http://www.nhs.uk/Conditions/Pilonidal-sinus/Pages/Treatment.aspx

It’s remarkable designed for me to have a web page,
which is beneficial for my know-how. thanks admin
Good way of explaining, and pleasant piece
of writing to obtain facts about my presentation topic, which
i am going to deliver in academy.