What is Osteitis Pubis?
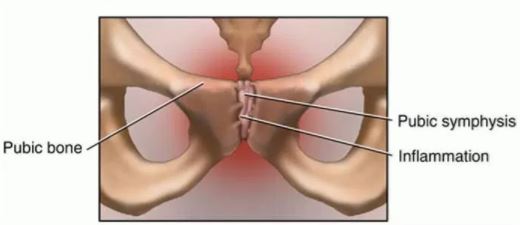
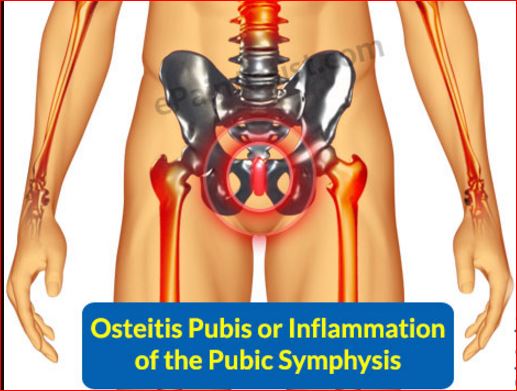
Osteitis pubis is a non-infectious inflammation of the pubic symphysis resulting to lower abdominal and groin pain. It is also known as pubic symphysitis.
The pubic symphysis is the cartilage where the left and right pubic bones meet and is responsible for absorbing force between the two. This joint is close to the body’s midline. It is a secondary cartilaginous joint meaning it is a joint that is made of hyaline cartilage as well as fibrocartilage. The pubic symphysis is enclosed by hyaline cartilage and joined by a disc made up of fibrocartilage.
Pubic symphysis Cartilage – Location and Function
A reinforcement of the fibrocartilage disc is made up of ligaments that attach to the disc itself. These ligaments also attach to the tendons from gracilis, rectus abdominis, and the obliquus externus.
In males, pubic symphysis is located above the penis and in females, it is located above the vulva. In males, this joint connects to penis ligaments and in females, the joint is found near the clitoris. In addition, in women, the area where there is connection of the pubic bones, it forms an opening in which a baby passes at time of birth.
During pregnancy and birth, ligaments surrounding the pubic symphysis tend to flex; this way, they allow a baby to pass without complications or difficulties. Normally, pubic symphysis joint can move two millimeters with a one degree rotation, but this flexibility changes and increases during birth.
When there is an inflammation (non-infectious swelling) of the pubic symphysis, it may be termed as pubic symphysitis or Osteitis pubis.
Sometimes, tissue damage is witnessed in patients with Osteitis pubis. It is mostly as a cause of invasive procedures around the pelvic area or inflammation processes in athletes. This condition is popular in ice skaters, long distance runners, dancers, footballers and weight lifters. This is so because certain muscles are attached to the symphysis.
When doing activities like running, these muscles contract exerting a certain force on the symphysis. Such actions did repeatedly end up injuring and damaging the symphysis.
Causes
The causes of Osteitis pubis can be classified into two; biomechanical inefficiency and overload or training errors. They include;
- Leg length differences
- Gait disturbance
- Pregnancy and child birth. During pregnancy, hormone relaxin is released to soften pelvic ligaments for labor. Falling, tripping, walking up stairs and strain when the ligaments are vulnerable can cause damage to the pubic symphysis. After childbirth, the ligaments may remain soft and be susceptible to injuries and damage.
- Bad running and walking methods
- Overuse
- Major trauma
- Gynecologic surgery that invades the pelvic girdle
- Repeated minor trauma
- Imbalance of the muscles
- Urologic surgery
- Rheumatologic disorders
- Working out on hard surfaces like concrete
- Using ill-fitting or worn off shoes
- Strenuous athletic activities
- Starting exercises after a long period of inactivity
- Intensifying workout procedures all of a sudden
- Working out on grounds that are uneven
- Stiff muscles in the buttocks, hips, and groin
- Pressure on athletes and footballers to have increased strength and big muscles, which compels them to over exert themselves when doing exercises
- Excessive contraction of abdominal muscles as a result of too many sit ups.
Signs and Symptoms
Among the signs and symptoms of Osteitis pubis are:
- A popping sensation when raising from a seat , walking on uneven grounds and turning in bed
- Fever
- Chills
- Weakness
- Pain in the front of the pelvic girdle (front and center of pubic bone). This pain then radiates outwards towards the thighs and groin.
- Unilateral lower abdominal pain around the pubic area
- Dull or sharp pain after certain activities such as running, kicking, changing direction, lying on a particular side, or raising a leg
- Pain when sneezing, coughing and climbing stairs
- Difficulty ambulating
- Rigors
- The patient experiences pain when squeezing in legs together or moving one apart from the other.
Diagnosis
Diagnosis is mostly done through physical examination. Laboratory results are useful only in determining the cause of the shearing forces to the pubic symphysis.
- The most specific diagnostic test is the direct pressure spring test. It involves palpating the pubic bone of the patient over their pubic symphysis. The physician then slides their finger a few centimeters to both sides laterally applying pressure. Pain suggests the patient has osteitis pubis.
- Checking the inguinal hernia
- Hip pain experienced in the longer leg in cases where patients have length differences discrepancies
- In cases where sacral innominate dysfunction is the cause, pain is experienced over sacroiliac joints
- Ultrasound of the pelvic girdle of the patient
- Computed tomography scan
- X-Ray

- Rectal examination
- Gynecologic exam
- Assessment of the weakness of hip adductors and flexors among other muscles in the region
- Erythrocyte sedimentation rate (ESR)
- Complete blood count (CBC)
- Blood culture in febrile patients
- Urinalysis
- Tenderness to palpation in the superior pubic ramus.
Treatment
Ice
Application of ice is known to be a home remedy for all sorts of inflammation. Applying ice reduces the swelling as well as the pain. The ice should however not be applied directly to the skin to avoid ice burns. Ice cubes or crushed ice can be wrapped in a towel or damp piece of cloth first, then applied on the inflamed area.
Physical therapy
This should be started for two main reasons; to alleviate the pain experienced by the patient and to correct certain mechanical problems that might, in the first place, be the cause of the Osteitis pubis.
Stretching exercises
The patient should participate in stretching exercises, but only when they are no longer experiencing pain.
Rest
Immobilization and bed rest to provide symptomatic pain relief and avoid further injuries.
Progressive ambulation
Practice progressive ambulation with the help of an assistive device.
Heat application
This is to relieve the symptoms. This is, however, done when the Osteitis pubis was detected late and the patient is no longer experiencing severe pain.
Other treatment regimes for Osteisis pubis are:
- Application of dynamic stabilization techniques
- The patient should use stair stepping machines to learn how to maneuver daily life activities like climbing up a flight of stairs
- The patient should have a workout schedule to exercise hip flexors, adductors, and other abdominal muscles
- Aquatic conditioning should be put in place
- Manipulation
- The patient should be put in electric stimulation sessions once pain caused by Osteitis pubis has subsided
- The physician incharge should administer non-steroidal anti-inflammatory drugs to ease the pain and inflammation
- Administering of steroids
- The patient can undergo prolotherapy with lidocaine and dextrose
- The patient can undergo strengthening therapy once they no longer experience pain caused by the condition
- In extremely severe cases, surgery can be put in place. Surgical procedures that are used in the treatment of Osteitis pubis include wedge resection, curettage, wide resection and arthrodesis.
- This is, however, very rare and has proven to have low success result rates.
Prevention
You may prevent Osteitis pubis by observing the following:
- Using proper shoes or footwear when working out or participating in sports. Proper footwear act as cushions of force exerted. They also provide support and stability when doing strenuous activities like kicking or running.
- Proper warming up before getting into strenuous exercises or activities to prepare the body for the intense exercise to follow shortly
- Doing exercises that help the muscles of the body stretch and grow in strength
- Adequate rest and recovery time
- Prohibiting and abstaining from doing exercises that cause pain or strain to the body.
Reference List
- Osteitis pubis. www.physioadvisor.com.au/injuries/hip-groin/oistetis-pubis/
- Symptoms of Osteitis pubis. www.leadingedgephysicaltherapy.com.au/common-conditions/groin-pain/oistetis-pubis/
- Prevention of Osteitis pubis. www.sportsinjuryclinic.net/sport-injuries/hip-groin-pain/oistetis-pubis
- Osteitis Treatment. www.stretchcoach.com/articles/oistetis-pubis/
- Pubic Symphysis. http://www.healthline.com/human-body-maps/pubic-symphysis
